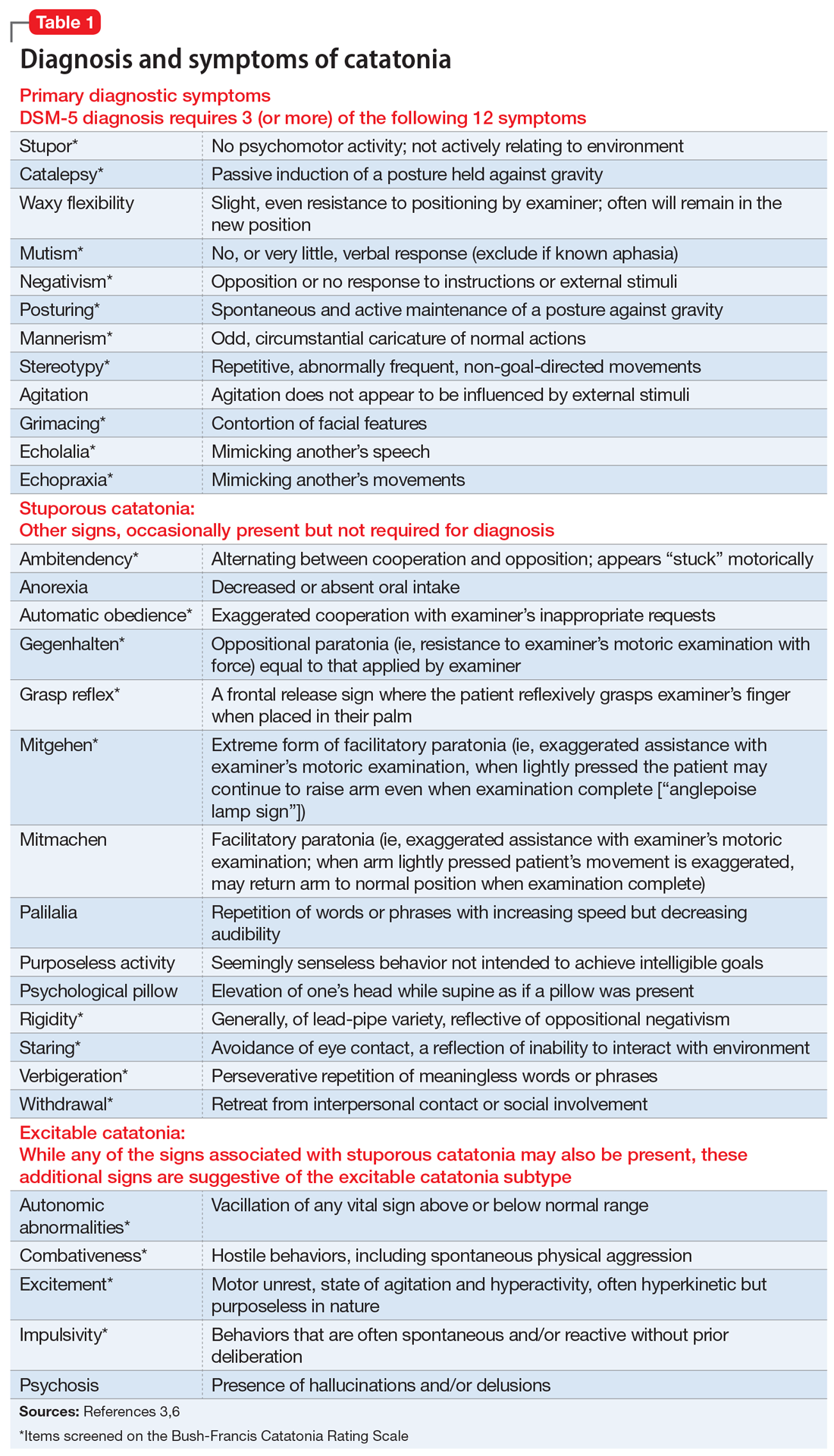
Mr. W, age 50, who has been diagnosed with hypertension and catatonia associated with schizophrenia, is brought to the emergency department by his case manager for evaluation of increasing disorganization, inability to function, and nonadherence to medications. He has not been bathing, eating, or drinking. During the admission interview, he is mute, and is noted to have purposeless activity, alternating between rocking from leg to leg to pacing in circles. At times Mr. W holds a rigid, prayer-type posture with his arms. Negativism is present, primarily opposition to interviewer requests.
Previously stable on paliperidone palmitate, 234 mg IM monthly, Mr. W has refused his past 3 injections. Past psychotropics include clozapine, 250 mg at bedtime (discontinued because Mr. W was repeatedly nonadherent to blood draws), risperidone long-acting injection, 25 mg every 2 weeks, as well as olanzapine, quetiapine, lurasidone, asenapine, lithium, fluoxetine, citalopram, mirtazapine (doses unknown). Previously, electroconvulsive therapy (ECT) was used to successfully treat his catatonia.
On the inpatient psychiatry unit, Mr. W continues to be mute, staying in bed except to use the bathroom. He refuses all food and fluids. The team initiates subcutaneous enoxaparin for deep vein thrombosis (DVT) prophylaxis and IV fluids for hydration. Mr. W receives a benzodiazepine challenge with lorazepam, 2 mg IM. Within 1 hour of receiving lorazepam, he is walking in the hall, speaking to staff, and eating. Therefore, lorazepam, 2 mg IM, 3 times a day, is continued, but the response is unsustained. Ultimately, ECT is initiated.
Continue to: Medical complications can be fatal