LEEP may have an adverse obstetric impact
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet. 2006;367:489–498.
Although most clinicians recognize that cold-knife conization has the potential to cause adverse obstetric outcomes, the same has not been recognized for loop electrosurgical excisional procedures (LEEP). In fact, most of the studies published in the early 1990s showed that LEEP had little impact on obstetric outcomes. Now we know better: Kyrgiou and colleagues conducted a systematic review and meta-analysis of the published literature on obstetric outcomes after treatment of CIN lesions, and found that all types of excisional procedures produce similar pregnancy-related morbidities.
LEEP had a significant association with preterm delivery (11% risk in treated women versus 7% in untreated women), low-birth-weight infants (8% in treated women versus 4% in untreated women), and premature rupture of membranes (5% in treated women versus 2% in untreated women). Although there were no significant increases in NICU admissions or perinatal mortality among the offspring of women who had undergone LEEP versus those who had not, nonsignificant increases were observed.
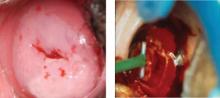
Similar increases in pregnancy-related morbidity were not observed among patients who underwent ablative procedures. This suggests that the amount of tissue that is removed during the LEEP (FIGURE 1) is important. Therefore, when treating CIN 2,3 lesions, especially in young women, consider using an ablative method such as cryotherapy or electrofulguration, unless colposcopy is unsatisfactory or there is a colposcopic or pathologic suspicion that an occult cancer is present.
FIGURE 1 CIN 2,3 and its treatment by LEEP
Is liquid-based cytology as sensitive as we thought?
Davey E, Barratt A, Irwig L, et al. Effect of study design and quality on unsatisfactory rates, cytology classifications, and accuracy in liquid-based versus conventional cervical cytology: a systematic review. Lancet. 2006;367:122–132.
Ronco G, Segnan N, Giorgi-Rossi P, et al. Human papillomavirus testing and liquid-based cytology: results at recruitment from the new technologies for cervical cancer randomized controlled trial. J Natl Cancer Inst. 2006;98:765–774.
Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, Wright TC Jr. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006;118:957–962.
A major reappraisal of liquid-based cytology (LBC) is under way. When it was first introduced, LBC was believed to provide a significant advantage over conventional cervical cytology in terms of sensitivity for CIN 2,3 or cancer. However, most of the studies that compared the 2 modalities had severe methodological problems. Many utilized historical controls, and most others simply reported increases in the number of cases cytologically diagnosed as squamous intraepithelial lesions (SIL). Very few measured histologic endpoints, and the few studies that did failed to blind the pathologists evaluating the histology to the cytologic findings. Only 1 small study was randomized.
Focus on high-quality studies finds lower sensitivity for LBC
Recently, Davey and colleagues conducted a systematic review of the published literature comparing LBC with conventional cytology. A total of 56 studies were evaluated, 52 of which provided enough information to evaluate differences between the 2 methods in the detection of low-grade squamous intraepithelial lesions (LSIL) and high-grade SIL (HSIL). These 52 studies included more than 1.25 million slides.
None of the studies that were evaluated were judged to be of “ideal quality,” and only 5 were judged to be of “high quality.” When all of the studies are taken into account and combined, there appears to be an increase in the cytologic detection of LSIL and HSIL with the use of LBC. However, further evaluation showed marked differences in the results obtained by studies of different quality.
When only “high-quality” studies are analyzed, there is no indication that LBC increases the detection of HSIL. Davey and colleagues concluded that there is no evidence that LBC reduces the proportion of unsatisfactory slides or outperforms conventional cytology in identifying women with CIN 2,3. They also noted that large randomized trials are needed.
Little difference between modalities in randomized trials
After the systematic review was conducted, 2 large trials comparing LBC with conventional cytology were published. In the first trial, Taylor and colleagues collected samples from South African women and analyzed them in blinded fashion in US laboratories. In their carefully controlled study, 5,652 women received either LBC or conventional cytology (rotated on a 6-month basis), and all women underwent colposcopy and cervical biopsy. No significant difference was observed in the sensitivity of LBC and conventional cytology in the detection of CIN 2,3 or cancer. In fact, there was a nonsignificant increase in sensitivity with conventional cytology, compared with LBC. Positive predictive value was lower with LBC than with conventional cytology. This means that a smaller proportion of women with an abnormal result on LBC had CIN 2,3 or cancer identified at colposcopy than did women who had an abnormal result on conventional cytology.