Results of a phase 2 trial suggest the multikinase inhibitor midostaurin can repair organ damage in patients with advanced systemic mastocytosis (SM).
The drug produced a 60% response rate among patients with mastocytosis-related organ damage, and the median duration of response was 24.1 months.
Fifty-six percent of patients required dose reductions due to toxic effects, but 32% of these patients were able to return to the starting dose.
Jason Gotlib, MD, of the Stanford University School of Medicine in California, and his colleagues conducted this study and reported the results in NEJM.
The study was funded by Novartis Inc., which manufactures midostaurin, also known as PKC412.
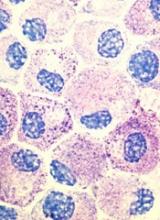
The researchers noted that roughly 90% of patients with advanced SM have a mutation known as D816V in the gene that encodes the protein KIT, which controls the growth of mast cells.
Unfortunately, the only drug approved to treat advanced SM in the US is the tyrosine kinase inhibitor imatinib, and this drug is not active against the mutated KIT D816V protein. Midostaurin, on the other hand, does inhibit KIT D816V.
With this in mind, Dr Gotlib and his colleagues set out to test midostaurin (given at 100 mg twice daily until disease progression or unacceptable toxicity) in 116 patients.
Eighty-nine of the patients had mastocytosis-related organ damage, 16 had aggressive SM, 57 had SM with an associated hematologic neoplasm, and 16 had mast cell leukemia.
Response
The median follow-up was 26 months (range, 12 to 54), and the study’s primary outcome was the best overall response.
The overall response rate for the primary efficacy population (the 89 patients with mastocytosis-related organ damage) was 60%. Forty-five percent of the patients had a major response, which was defined as complete resolution of at least one type of mastocytosis-related organ damage.
The overall response rate was 75% for patients with aggressive SM, 58% for SM patients with an associated hematologic neoplasm, and 50% for patients with mast-cell leukemia.
Responses occurred in all subgroups, which included patients who were positive for KIT D816V.
The researchers noted that responding patients were less likely to need red blood cell or platelet transfusions, experienced improvements in liver function, and had fewer signs of malabsorption such as weight loss.
The median duration of response for all responders in the primary efficacy population (n=89) was 24.1 months.
Survival
The median overall survival was 28.7 months in the primary efficacy population (n=89) and 33.9 months in the intention-to-treat population (n=116). The median progression-free survival was 14.1 months in the primary efficacy population.
The survival benefit among patients with mast cell leukemia was particularly striking, according to Dr Gotlib. Although most people succumb to this form of the disease within 6 months of diagnosis, the median overall survival of midostaurin-treated patients with mast cell leukemia was 9.4 months.
The median overall survival was not reached among patients with aggressive SM and was 20.7 months among patients who had SM with an associated hematologic neoplasm.
Safety
The most common nonhematologic adverse events were nausea (79%), vomiting (66%), and diarrhea (54%). The most common grade 3/4 nonhematologic adverse events were fatigue (9%) and diarrhea (8%).
Grade 3/4 hematologic adverse events included new or worsening neutropenia (24%), anemia (41%), and thrombocytopenia (29%).
Researchers reduced the dose of midostaurin in 65 patients (56%), mostly due to adverse events (n=48). Twenty-one of these patients (32%) were later able to return to the initial dose.
Eighty-four patients (72%) discontinued treatment, and 32 (28%) were receiving ongoing treatment at the time of data cutoff. The most frequent reasons for treatment discontinuation were disease progression (33%) and adverse events (22%).
Compassionate use
The phase 2 study results are reinforced by a letter published in the same issue of NEJM, which describes a compassionate use program for midostaurin in advanced SM.
The letter includes results in 28 patients. After a median follow-up of 18.5 months, the overall response rate was 71%. The overall survival rate was 42.7%.
The most frequent adverse events were nausea/vomiting in 89% of patients (leading to failure/discontinuation in 18%), lymphocytopenia in 61% (without opportunistic infection), and photosensitivity in 25%.