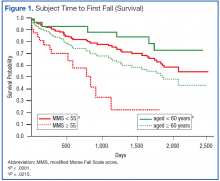
Grouping subjects by MMS alone yielded significantly divergent survival curves only for cutoffs of MMS ≥ 40, ≥ 50, ≥ 55 (log-rank statistic P = .0061, P = .0002, and P < .0001, respectively). Figure 1 (red) shows the difference in survival for MMS ≥ 55 vs MMS < 55, where the mean time to fall was 701 ± 88 days for those with a MMS ≥ 55 compared with 1,628 ± 65 days for MMS < 55.
When age cutoff alone (using 5-year age intervals) was used to construct fall survival curves, only breakpoints of age ≥ 60, ≥ 75, and ≥ 80 years yielded significantly divergent curves (log-rank statistic P = .0215, P = .0264, and P = .011, respectively). Figure 1 (green) shows the difference in survival for subjects aged < 60 years vs aged ≥ 60 years.
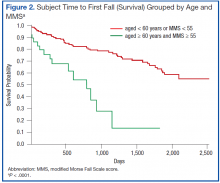
The hypothesized combined cutoff of subjects aged ≥ 65 years and MMS ≥ 55 yielded divergent survival curves (log-rank statistic of P = .0011). However, survival curves based on a cutoff of subjects aged ≥ 60 years and ≥ 55 MMS yielded the most statistically significant separation (logrank statistic P < .0001) (Figure 2). Subjects aged < 60 years or with a MMS < 55 had a mean survival of 1,634 ± 65 days; whereas those aged ≥ 60 years and a MMS ≥ 55 had a mean survival of 668 ± 90 days.
A notable similarity of the survival curves for MMS ≥ 55 vs MMS < 55 compared with those based on a cutoff of subjects aged ≥ 60 years and ≥ 55 MMS is observed in comparing Figures 1 (red) and 2. The log-rank statistic chi-square values are 17.44 and 22.75, respectively, suggesting the separation of subjects by a combination of age and MMS yields a more robust divergence in outcomes than does separation by MMS alone.
Discussion
This retrospective chart review evaluated the utility of a MMS combined with age in predicting the risk of patients with AF experiencing serious falls following hospital discharge. When used alone, the MMS separates those at relatively low and high risk of subsequent falls requiring acute medical care. When combined with the factor of patient age, this separation improves and is most predictive for the group of AF patients aged ≥ 60 years with a MMS of ≥ 55. Half of this group had fallen 668 ± 90 days after discharge; whereas those aged < 60 years or with a MMS < 55 did not reach the point of 50% falling until 1,634 ± 65 days after discharge. Age alone allows a statistically significant differentiation of fall risk, but less so than does the MMS alone or the MMS combined with age.
Assessing fall risk can be as simple as asking whether a patient has fallen during the previous year or has a problem with balance or gait, or it can be as complex as an in-depth investigation of physical, cognitive, pharmacologic, environmental, and social factors.12,13 Beyond the parameters of validity and discrimination power, a predictive tool must be easy to use. Within the VA hospital system, where the MFS is a part of every nursing intake assessment, a MMS can be obtained within seconds from the EMR. This, coupled with the patient’s age, allows the provider to immediately identify those patients with AF who are at high risk for serious falls following hospital discharge.