It is important to note that although a positive bronchodilator response is highly suggestive of asthma in the appropriate clinical circumstance, it is not required for diagnosis, and inhaled bronchodilators may be useful in disease management even in the absence of a positive response. Patients with nonspecific reductions in the FVC, with symptoms not consistent with asthma, or not responding to typical asthma therapy are more likely to have been falsely diagnosed. These patients should have lung volumes and diffusion capacity of carbon monoxide measured to evaluate for other potential etiologies (eg, parenchymal lung disease, pulmonary vascular disease). 4
Bronchoprovocation testing is useful for demonstrating airway hyperresponsiveness in a patient with symptoms suggestive of asthma, particularly those with normal baseline spirometry. Patients should have testing performed and interpreted in accordance with ATS
standards.8 Although methacholine challenge testing is preferred, other methods including cold air or eucapnic hyperventilation are also established. Exercise challenge testing, although less sensitive, remains a useful tool, particularly in patients with primarily exertional symptoms. It is important to note that a positive bronchoprovocation test result may occur in other conditions. Whereas a positive test is consistent with asthma, a negative test may be more useful to exclude the diagnosis .8 Finally, chest imaging with plain film radiographs (posteroanterior and lateral views) is important to exclude parenchymal lung disease or mediastinal disorders. Further imaging with computed tomography is not indicated in the absence of atypical clinical features (such as abnormal plain films or failure to respond to therapy).
Management
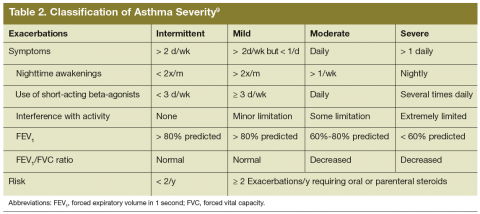
The initial management of asthma in based on severity and follows a stepwise progression according to the 2007 National Asthma Education and Prevention Program. 9 Severity is determined by the following factors: symptoms in the past 2 to 4 weeks, pulmonary function testing, and number of exacerbations requiring oral glucocorticoids (Table 2).
The initiation of therapy is based on the assessment of severity (Table 3). Patients with intermittent asthma are treated initially with short-acting beta-agonists (SABA) alone. Patients with known triggers are instructed to use beta-agonists about 20 minutes prior to a known trigger such as exercise. 4,9 For a patient with mild persistent asthma, the preferred controller medication is a low-dose inhaled corticosteroid (ICS). If a patient has moderate persistent asthma, the preferred controller medication becomes a lowdose ICS plus a long-acting beta agonist (LABA) or a medium-dose ICS. Severe persistent patients are treated with a medium-dose ICS and a LABA or a high-dose ICS. 4,9 In patients who need additional therapy beyond that described here, providers may consider adjunctive therapy with theophylline, leukotriene receptor antagonists (such as montelukast), or cromolyn/nedocromil. 4,9 If a patient has severe persistent asthma, anti-IgE therapy omalizumab can be considered if serum IgE levels are within the established range (30-700 IU/mL). 10
Chronic asthma management relies on assessment and monitoring of functional impairment and response to therapy over time. Impairment is best assessed using a validated questionnaire assessing nighttime awakenings; frequency of as-needed bronchodilator therapy; limitation in home, school, or work activities; and perception of control or peak flow monitoring. 4 One questionnaire that has been validated in the outpatient setting (as well as for home use via mail or telephone) is the Asthma Control Test. 11-14 The history obtained in clinic should assess risk factors for future exacerbations, such as the use of oral glucocorticoids, emergency department visits, hospitalizations, and admissions to the intensive care unit. For patients whose symptoms are not well controlled, a step up in therapy of one level should be performed. Therapy can be continued or stepped down (to minimize adverse effects) in those with adequate control.