Data analysis
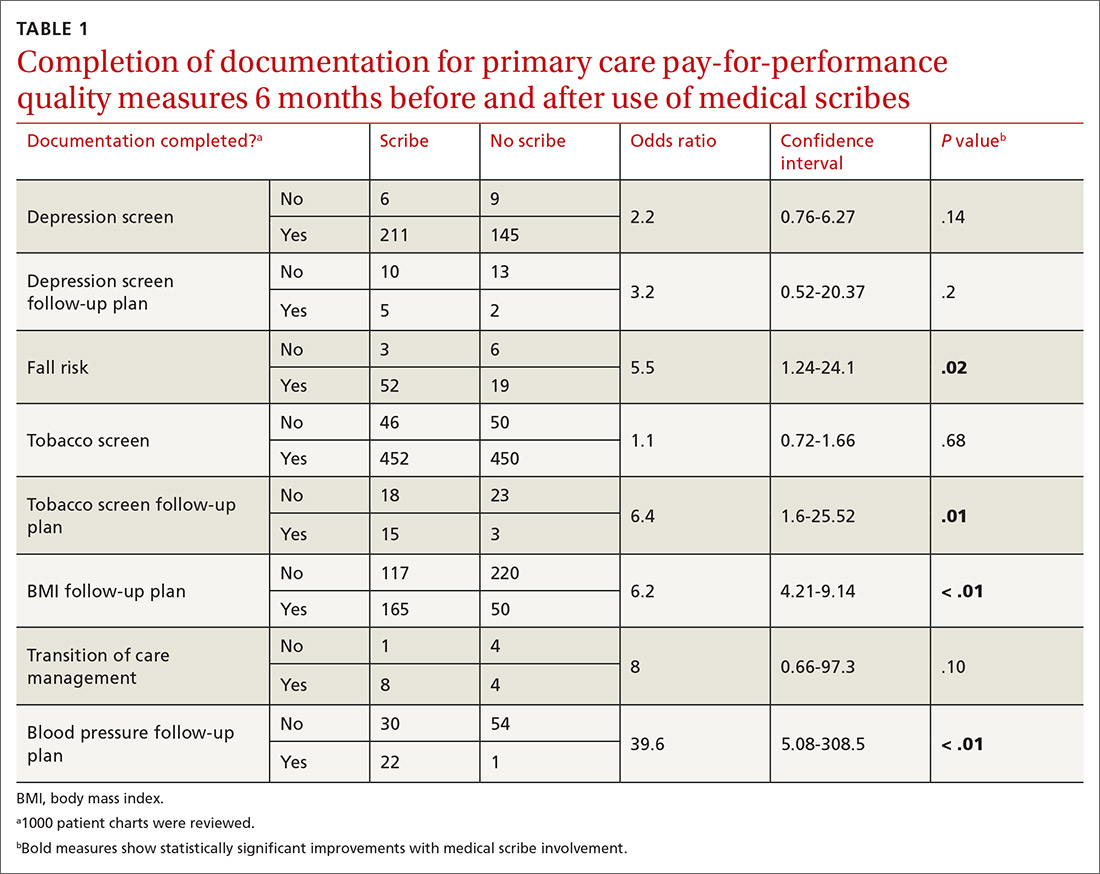
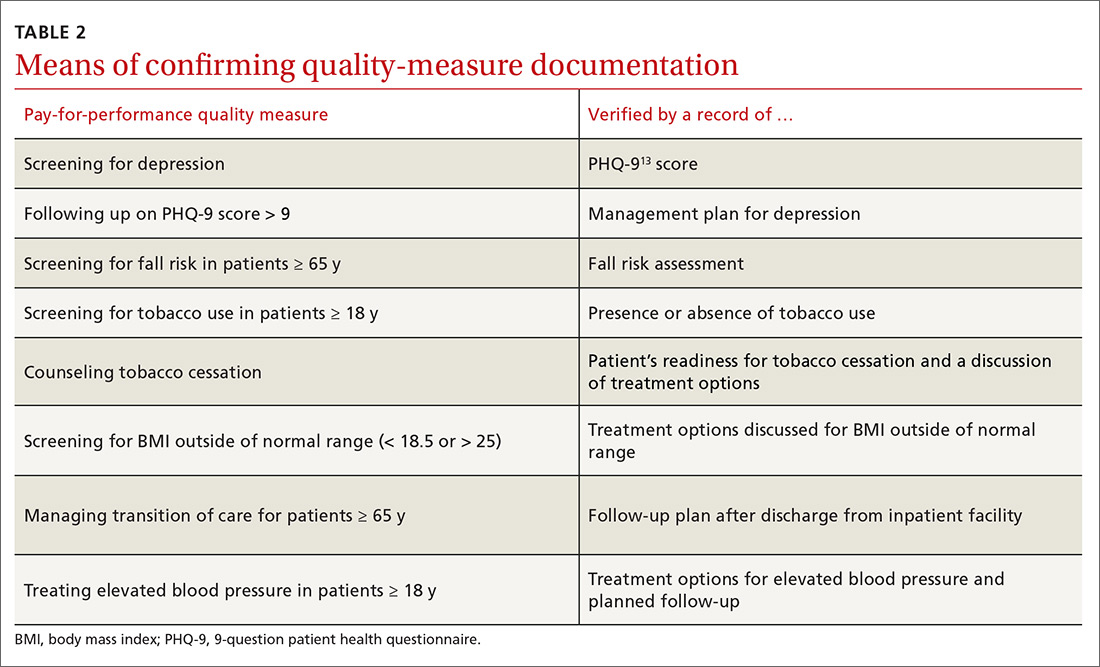
During chart review, we assessed the rate at which documentation was completed for 8 quality outcome measures commonly used in the primary care setting (TABLE 1), before and after the introduction of medical scribes. These quality measures and pertinent descriptors are listed in TABLE 2.13 Presence or absence of documentation on all quality measures was noted for all applicable patients.
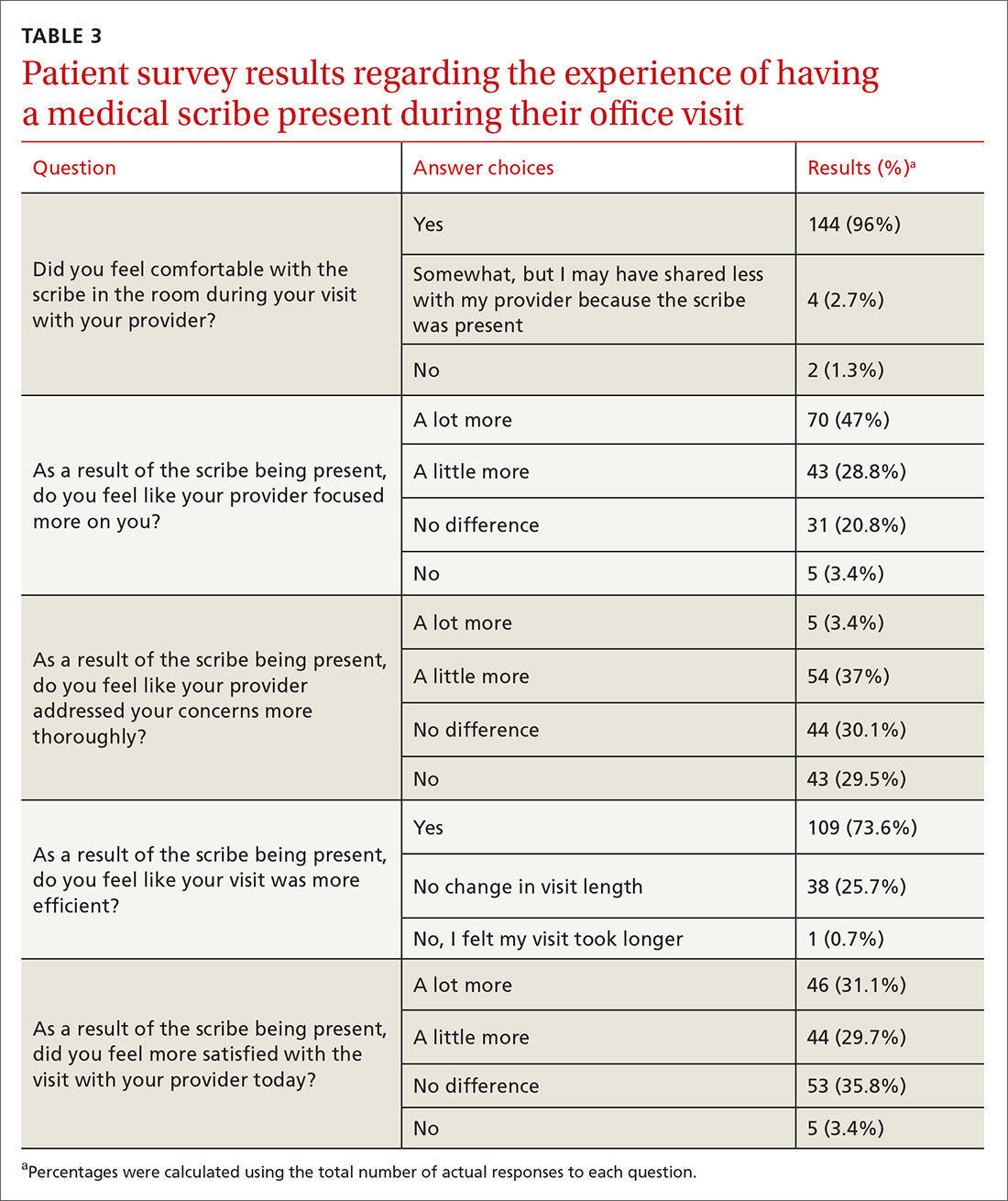
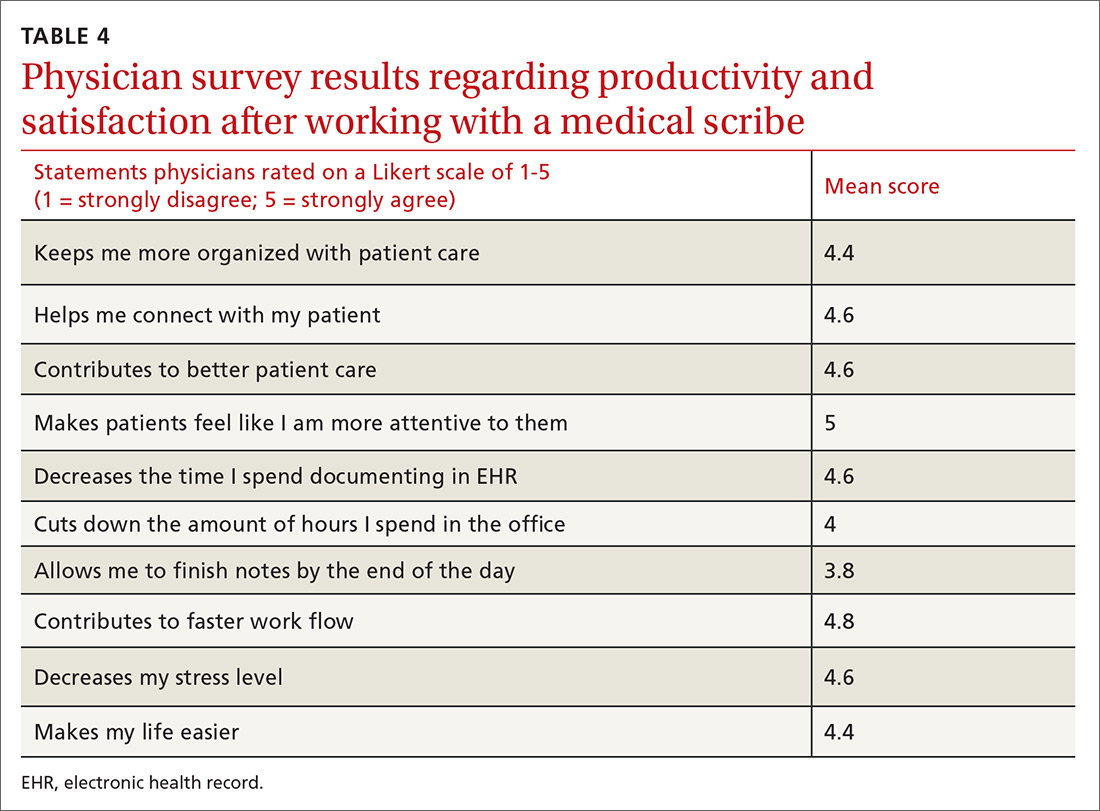
One hundred fifty patients were surveyed immediately after their office visit on their perceptions of medical scribes, including their attitude toward, comfort with, and acceptance of medical scribes (TABLE 3). Five participating physicians were surveyed to assess their perceptions related to productivity and job satisfaction with the use of medical scribes (TABLE 4), and regarding time saved and additional patients seen. Those who collected and analyzed the data from the surveys were blinded to patient and physician identifiers.
Statistical analysis
Using chi-squared tests, we compared the number of positive documentations for the 8 outcome measures before and after the use of medical scribes. Two-sided P values < .05 were considered statistically significant. All statistical analyses were performed with the use of STATA version 9 (StataCorp LP. College Station, Tex).
Physician survey data were calculated on a Likert scale, with a score of 1 corresponding to “strongly disagree,” 2 “disagree,” 3 “neither agree nor disagree,” 4 “agree,” and 5 “strongly agree.” Using the 5 answers generated from the 5 physicians, we calculated the mean for each question.
RESULTS
The use of scribes demonstrated a statistically significant improvement in the documentation of 4 (out of 8) pay-for-performance measures (TABLE 1): fall risk assessment (odds ratio [OR] = 5.5, P = .02), follow-up tobacco screen (OR = 6.4; P = .01), follow-up body mass index (BMI) plan (OR = 6.2; P < .01), and follow-up blood pressure plan (OR = 39.6; P < .01). Sample sizes of each quality measure vary as there were differing numbers of applicable patients for each quality measure within the overall 1000 charts.
Continue to: We established at the beginning...