Case
A 63-year-old woman with multiple medical conditions presented to the ED with abdominal distention, pain, and 4-day history of fever. Physical examination revealed a distended but nontender abdomen. Her vital signs included a fever of 103.1°F, tachycardia, tachypnea, and a blood pressure of 101/69. To further evaluate the abdominal distention, supine abdominal radiographs were obtained (Figure 1a and 1b).
What is the differential diagnosis?
What would be the most appropriate next imaging test?
Answer
The abdominal radiographs demonstrated a nonobstructed bowel gas pattern—ie, there were no dilated loops of small or large bowel (>3 cm or >7 cm, respectively). Although limited by supine position, there was no evidence of perforation as no signs of free air were visualized. There was a large amount of stool within the large bowel, appearing on radiographic images as the mottled air and soft-tissue density (white asterisks, Figure 2a and 2b).
Although bowel obstruction had been ruled out in this patient, the differential for abdominal pain with fever remained wide, predominately for infectious and inflammatory conditions (eg, appendicitis, diverticulitis, inflammatory bowel disease, other forms of colitis/enteritis, pancreatitis, abscess, mesenteric).In cases such as the one presented, the most appropriate next imaging examination would be a computed tomography (CT) scan with both oral and intravenous (IV) contrast. Oral contrast is useful since several of the conditions in the differential diagnosis require evaluation of the bowel wall and, in cases of suspected abscess, it assists in differentiating a collection from adjacent loops of bowel. Intravenous contrast is useful to evaluate for inflammation and assessing the bowel.
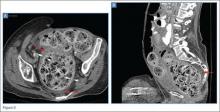
In this case, an abdominal CT was performed, using both oral and IV contrast. Axial and sagittal images demonstrated a large amount of stool in a distended rectum (white asterisks, Figures 3a and 3b), thickening of the rectal wall (white arrows, Figures 3a and 3b), and stranding of the perirectal fat indicative of perirectal inflammation (red arrows, Figures 3a and 3b). Based on these findings, the patient was diagnosed with stercoral colitis.
Stercoral colitis is inflammation of the colonic or rectal wall secondary to increased intraluminal pressure caused by impacted fecal material. This condition is most common in elderly patients and bedridden patients with chronic constipation. As this case illustrates, the clinical presentation of stercoral colitis is nonspecific, with wide range of symptoms including constipation, abdominal distention, vomiting, abdominal tenderness, peritonitis, fever, and sepsis.1
While rectal examination can confirm fecal impaction, a lack of palpable fecaliths does not exclude impaction, since fecaliths may be proximal to the palpable area. In addition, abdominal radiographs typically show nonspecific findings, such as heavy fecal burden and colonic dilation (eg, distension localized to the rectosigmoid region or pancolonic region).1 Therefore, in cases of suspected stercoral colitis, it is important to examine radiographs for signs of perforation, such as free air; however, due to low sensitivity, absence of free air on abdominal X-ray does not rule out pneumoperitonium.2Computed tomography of the abdomen and pelvis is the most reliable test for detecting stercoral colitis and its associated complications. Characteristic findings, as seen in the presented patient, include a large dense mass of fecal material, focal or diffuse thickening of the colonic wall, and pericolonic fat-stranding that affects the impacted region. When ulceration or perforation occurs, CT will reveal and extra luminal gas and/or abscess.1,3
Since stercoral colitis is associated with a reported mortality rate of 32% to 57%, with death often occurring within the first 24 hours from presentation, rapid diagnosis is essential.1 Once diagnosed, stercoral colitis is treated with aggressive fecal disimpaction, hyperosmolar enema, and, when indicated, surgery. The patient in this case was admitted for treatment. Unfortunately, despite all appropriate therapy efforts, she succumbed due to medical complications of her underlying illnesses.
Dr Belfi is an assistant professor of radiology at Weill Cornell Medical College in New York City, and an assistant attending radiologist at New York-Presbyterian Hospital/Weill Cornell Medical Center. Dr Hildick-Smith is a medical student at Weill Cornell Medical College in New York City. Dr Hentel is an associate professor of clinical radiology at Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology at New York-Presbyterian Hospital/Weill Cornell Medical Center; and associate editor, imaging, of the EMERGENCY MEDICINE editorial board.