Case Reports

Cutaneous Leishmaniasis: An Emerging Infectious Disease in Travelers
Leishmaniasis describes any of 3 diseases caused by protozoan parasites of the genus Leishmania, the most common of which is cutaneous...
Dr. Anderson is from the Department of Dermatology, Wake Forest University School of Medicine, Winston-Salem, North Carolina. Dr. Minni is from Water’s Edge Dermatology, Stuart, Florida. Dr. Nowak is from Palm Beach Dermatology, West Palm Beach, Florida. Dr. Karai is from Aurora Diagnostics, Miami Lakes, Florida. Dr. Sanik is from Larkin Community Hospital, Miami, Florida.
The authors report no conflict of interest.
Correspondence: Kathryn L. Anderson, MD, Medical Center Blvd, Winston-Salem, NC 27157 (Anderson.kathryn.lee@gmail.com).

Hansen disease, also known as leprosy, is a chronic granulomatous infectious disease that is caused by Mycobacterium leprae. We report an unusual case of a 65-year-old man who presented with multiple anesthetic, annular, erythematous, scaly plaques with a raised border without any known exposures to leprosy. Histologic examination revealed a perineural lymphohistiocytic infiltrate and rare bacilli demonstrated on Fite staining. After confirmation with polymerase chain reaction (PCR) and consultation with the National Hansen’s Disease Program (Baton Rouge, Louisiana), the patient was placed on a regimen of rifampicin 600 mg once monthly and dapsone 100 mg once daily for 6 months, which showed considerable improvement. This case demonstrates the identification of leprosy in central Florida, a region that is not known to be endemic to the disease. Leprosy, however rare, must be part of a practitioner’s differential diagnosis even without history of traditional exposures.
Practice Points
A 65-year-old man presented with multiple anesthetic, annular, erythematous, scaly plaques with a raised border of 6 weeks’ duration that were unresponsive to topical steroid therapy. Four plaques were noted on the lower back ranging from 2 to 4 cm in diameter as well as a fifth plaque on the anterior portion of the right ankle that was approximately 6×6 cm. He denied fever, malaise, muscle weakness, changes in vision, or sensory deficits outside of the lesions themselves. The patient also denied any recent travel to endemic areas or exposure to armadillos.
Biopsies were taken from lesions on the lumbar back and anterior aspect of the right ankle (Figure 1A). Hematoxylin and eosin staining revealed a granulomatous infiltrate spreading along neurovascular structures (Figure 2). Granulomas also were identified in the dermal interstitium exhibiting partial necrosis (Figure 2 inset). Conspicuous distension of lymphovascular and perineural areas also was noted. Immunohistochemical studies with S-100 and neurofilament stains allowed insight into the pathomechanism of the clinically observed anesthesia, as nerve fibers were identified showing different stages of damage elicited by the granulomatous inflammatory infiltrate (Figure 3). Fite staining was positive for occasional bacilli within histiocytes (Figure 3A inset). Despite the clinical, histologic, and immunohistochemical evidence, the patient had no known exposure to leprosy; consequently, a polymerase chain reaction (PCR) assay was ordered for confirmation of the diagnosis. Surprisingly, the PCR was positive for Mycobacterium leprae DNA. These findings were consistent with borderline tuberculoid leprosy.
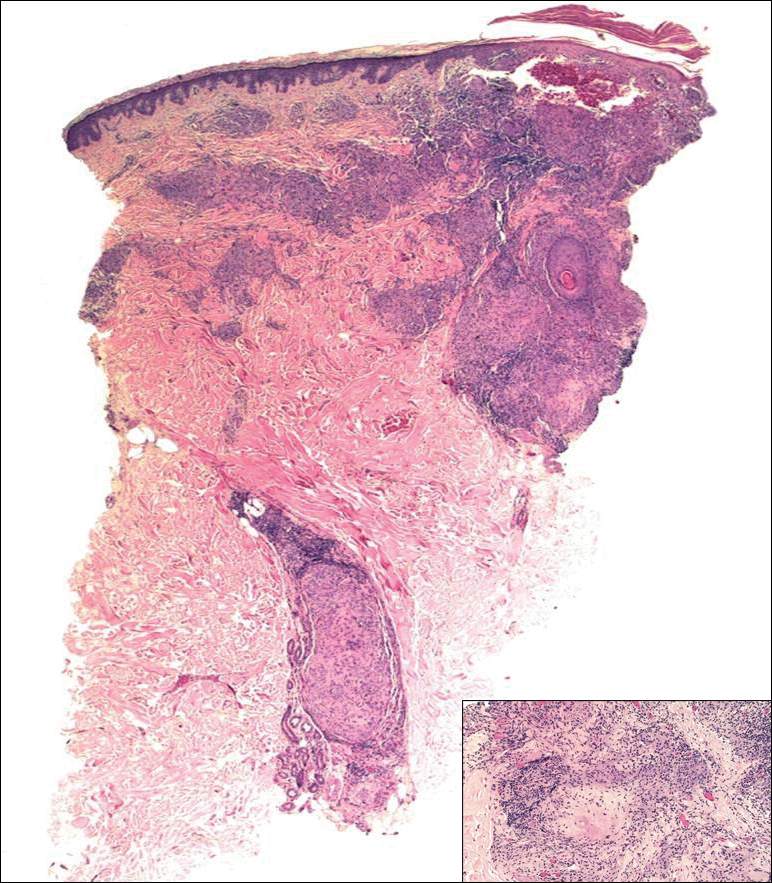
Figure 2. Hansen disease histopathology showed a superficial and deep focally necrotizing granulomatous infiltrate following neurovascular bundles and adnexal structures (scanning view)(H&E, original magnification ×20). The inset shows granulomas located in the interstitial dermis (H&E, original magnification ×100).
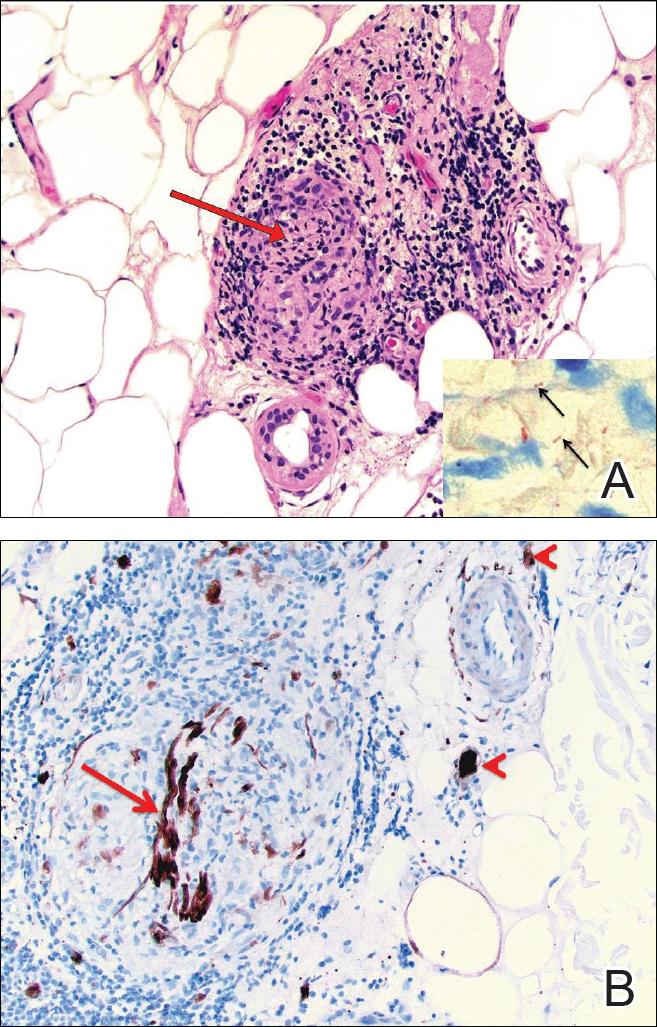
Figure 3. Perineural granulomatous inflammatory infiltrate in Hansen disease (red arrow pointing to nerve)(A)(H&E, original magnification ×400). The inset shows Fite-positive rod-shaped bacteria (black arrows). S-100 stain highlighted a disrupted nerve within the granuloma (red arrow) and nearby intact nerves (red arrowheads)(B)(original magnification ×40).
The case was reported to the National Hansen’s Disease Program (Baton Rouge, Louisiana). The patient was started on rifampicin 600 mg once monthly and dapsone 100 mg once daily for 6 months. The lesions exhibited marked improvement after completion of therapy (Figure 1B).

Leishmaniasis describes any of 3 diseases caused by protozoan parasites of the genus Leishmania, the most common of which is cutaneous...

Leprosy is a chronic granulomatous infection caused by the organism Mycobacterium leprae that primarily affects the skin and peripheral nerves.
Hansen disease, also known as leprosy, is a chronic inflammatory disease caused by Mycobacterium leprae and Mycobacterium lepromatosis. The mode...
