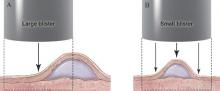
Figure 2. Punch biopsy of subepidermal blisters. Cross-sectional view showing sampling of a large blister with approximately 75% of the sample representing perilesional skin (A) and a small blister with at least 3 mm of perilesional skin included in the specimen (B). Illustration by Kyle Cunningham, Biomedical Illustration Services at the University of Mississippi Medical Center (Jackson, Mississippi).
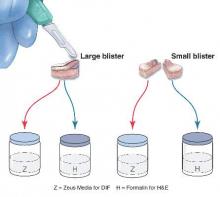
Figure 3. Punch biopsy of subepidermal blisters. Specimens from large blisters are bisected at the bedside with a no. 15 blade following the line drawn previously to ensure that perilesional skin and the “take-off point” of the blister will be visible when the cut edge is properly embedded in the laboratory. Excisional punch biopsies of small blisters are simply bisected. Half of each specimen is placed in formalin for hematoxylin and eosin processing, and half is placed in Zeus (or Michel) medium for direct immunofluorescence. Illustration by Kyle Cunningham, Biomedical Illustration Services at the University of Mississippi Medical Center (Jackson, Mississippi).
The second method is to choose any intact tense blister20,24 and, utilizing a surgical marker, draw a line from the roof of the blister onto the adjacent perilesional skin (Figure 1). After blotting with an alcohol pad so as not to remove the mark, anesthetize the site with lidocaine 1% with epinephrine,24 then take an 8-mm punch biopsy encompassing 75% perilesional skin and 25% of the blister centered on the line (Figure 2). After separating the punch specimen from the subcutaneous tissue with surgical scissors, hold the tissue with forceps and bisect the specimen with a no. 15 scalpel blade. Use a sawing motion along the line drawn in the prior steps (Figure 3). Submit half of the biopsy for H&E staining in formalin and the other half for DIF in Zeus medium.
Advantages
This approach offers several advantages. First, the technique requires only 1 invasive procedure, not 2 separate biopsies, so that the procedure can be done quickly and efficiently with the least morbidity and scarring. Secondly, because the patient is billed for 1 biopsy instead of 2, the single punch biopsy technique is more cost effective.
The bisected specimen resulting from complete excision of a small blister or from biopsy of a larger blister that includes 75% perilesional skin and 25% from the blister cavity also provides the best tissue specimen for interpretation of the subepidermal blistering processes via H&E staining.4,20,24 When traditional unmarked punch specimens of a blister margin are sent to the laboratory in formalin for H&E staining, the technician that grosses the specimen may or may not bisect the specimen showing the “take-off” point of the blister.
Finally, when the DIF specimen is prepared using either of these 2 approaches, the immunoprecipitants can be seen at the dermoepidermal junction or in the papillary dermis in the perilesional portion of the specimen.2,4 Additionally, the immunoprecipitant may be identified on the roof or floor of the blister. Although this approach has not been studied in a systematic fashion, we believe this technique provides “bonus” information to help differentiate BP and EBA correlating with salt-split skin blisters produced for indirect immunofluorescence.5,6
Limitations
It is critical for the pathologist or technician grossing these specimens to understand the techniques that are being employed and to ensure that the submitted half punch specimens are embedded so that the flat surface is cut so that the edge of the blister is properly sectioned for both H&E and DIF specimens. Additionally, with either recommended technique, if the portion of perilesional skin is not sufficient and the epidermis completely separates from the dermis, interpretation of both the H&E staining and DIF sections is substantially compromised.20 Therefore, an 8-mm disposable punch is recommended to avoid mangling the specimens when they are bisected and to insure that the epithelium is not lost. This technique is less suitable for blistering processes with a positive Nikolsky sign, such as pemphigus and toxic epidermal necrolysis, because the small area of perilesional skin adjacent to the blister may detach completely, requiring the epidermis and dermis to be evaluated separately or, in the worst-case scenario, the epidermis may be lost in processing.
Conclusion
Bisecting a single punch biopsy on subepidermal blisters provides the best specimen for H&E staining and DIF. The single punch biopsy technique also differentiates BP and EBA without utilizing salt-split skin immunofluorescence studies. This technique is more efficient and cost effective than the traditional approach of multiple biopsies on subepidermal blisters.

