The Role of Serologic Testing
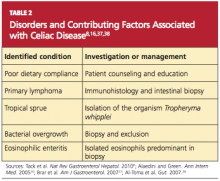
Current data demonstrate that autoimmune diseases are on the rise,8,16,36 and CD can be the primary cause or a contributing factor in several other disorders (see Table 28,16,37,38). Gastroenterologists may be correct in stating that biopsy is the only way to make a diagnosis of CD or to stage CD-associated intestinal damage4,26; yet by implementing a protocol of serologic testing for tTG and EMA in at-risk patients, PCPs could prevent a missed diagnosis on EGD when biopsy has not been considered, as in the case of atypical CD; or when biopsy results are negative in a patient with latent CD.39,40
Because of its high negative predictive value, serologic testing should be conducted first to significantly reduce the probability of suspected CD. Such selective screening should be performed by the PCP before invasive testing by the gastroenterologist and before long-term empiric treatment for idiopathic GERD, IBS, or other unexplained disorders.32,40
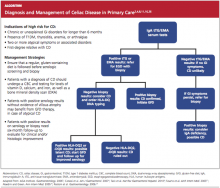
Thus, it has been recommended that PCPs perform screening for CD in patients with unexplained chronic GI disturbances or a familial prevalence of CD, or in those who present with the atypical signs of CD or with associated disorders.1,10,16,20 Whether serologic screening results are positive or negative for CD, the patient with classic GI symptoms should undergo endoscopy with biopsy to confirm active disease and to evaluate the extent of intestinal damage—or to explore other causes.26,39 An algorithm2,4,8,11,16,26 illustrating suggested screening, treatment, and follow-up strategies for patients at high risk for CD is shown below.
Catassi and Fasano34 recently proposed a “four out of five” rule, by which diagnosis of CD may be confirmed in patients with at least four of the following five criteria:
• Typical symptoms of CD
• Positive serology (ie, IgA tTG and IgA EMA antibodies)
• Genetic susceptibility (as confirmed by the presence of HLA-DQ2 and HLA-DQ8)
• Small intestine biopsy results indicating celiac enteropathy
• Improvement of CD signs and symptoms following implementation of the GFD.34
CURRENT TREATMENT AND ASSOCIATED CHALLENGES
Because gluten consumption is the principal trigger of CD pathology, a GFD is considered the safest, most effective therapy for the disorder.1,8,10,11,16,19 Implementing and maintaining the GFD involves a considerable learning curve for the patient, the patient’s family, and possibly the provider; to achieve complete recovery, all involved must become knowledgeable regarding gluten-free and gluten-containing products. The patient must be willing and able to avoid those that contain gluten and bear the potentially high costs8 of gluten-free foods.
Even for patients with CD who are determined to comply with the GFD, gluten monitoring can be difficult. There are ways to determine what is a safe level of gluten ingestion for each patient, but trace amounts of gluten are found in many products, including some that are marked “gluten-free.”1,41 The FDA has proposed that a product labeled gluten-free may contain no more than 20 parts per million (ppm, ie, 20 mg/kg) of gluten.42 In other countries, however, acceptable levels may be as high as 200 ppm (200 mg/kg)—which are considered well above the trigger amounts in the average patient with CD.1,41 The complex nature of each patient’s sensitivity to gluten and the ubiquitous presence of gluten as a food source in both industrialized and developing countries make adherence to the GFD challenging.10
It is critical for the PCP to help the patient review all of his or her prescription and OTC pharmaceuticals and nutritional supplements, as these may contain hidden gluten in the form of modified starches and other fillers.41 It may be also advisable to involve the patient’s pharmacist, requesting an assessment for agents that may be suspect.
A management team approach may ensure the most integrative care. In addition to the PCP and the pharmacist, such a team might include a gastroenterologist, an endocrinologist, a nutritionist, and a psychologist, who may be needed to help the patient confront the great life adjustment required, in addition to addressing other behavioral disorders that are common in patients with CD.10,26
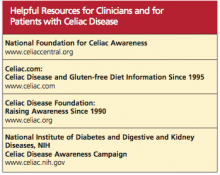
See the box for resources that may be beneficial for both patients and their clinicians.
Alternative Medicine Options
Alternative medicine is gaining favor, especially when no drug therapy is currently available to alleviate gluten toxicity. Supplementation with the fat-soluble vitamins (A, D, E, and K), vitamin B12, folic acid, and the minerals calcium and iron, as indicated by serum deficiencies, is recommended.10,20 Supplementation with digestive enzymes, which are known to be deficient in patients with CD as a result of villous atrophy, may help break down undigested gluten proteins; research is under way to find a recombinant enzyme therapy.10 Researchers have recently shown that probiotics (specifically, Bifidobacterium lactis) significantly reduce the immune response when incidental exposure to gluten occurs.43